Still Naked…
Posted: August 20, 2018 Filed under: Change, Disruptive Behavior, Energy, Heretic, Leadership, Safety, speaking up | Tags: Accountability, brave, Hospitals, Leadership, Patient Experience, speaking up, taking risks 1 CommentIt’s been more than five years since I dipped my toe into the world of blogging when I wrote – “The Emperor is Naked! Taking risks to reduce risk…”
The title was a clumsy headline intended to grab your attention.
The point then is the same as it is today so here’s a reprise – Still Naked
The fear of speaking up and being vulnerable is getting in the way of delivering safe and effective healthcare. The fear of speaking up is paralyzing leaders and their teams.
Coming over that fear requires bravery and as my friend and mentor Steve Farber (author of the Radical Leap) would say, vulnerability:
“Vulnerability aids human connection, and connection is the conduit for energy. Pretense of invincibility builds walls and creates distance between human hearts.”
Time to close this distance. Time to speak up. Time to get naked…
Grassroots Change + Personal Accountability in Healthcare
Posted: March 20, 2015 Filed under: Accountability, Change, Disruptive Behavior, Heretic, Leadership, Learning, Love, Making a Difference, Patient Experience, Personal Accountability, Perspective, Safety, Trust, Workplace Culture 1 CommentChange and personal accountability in health and care!
Standing on the shoulders of the rebels, the crazy ones, the trouble makers and the boat rockers – these are the folks that I am blessed to call my friends and my colleagues; these are the people that push the envelope for change, that embrace the hard work and the ones I love!
Here’s to Colin Hung, Linda Galindo, Helen Bevan, Tracy Granzyk, Dave Mayer, Michael Bennick, Paul Westbrook, Paul Levy, Katy Schuler, Steve Farber, Jake Poore, Diana Christiansen, Jason Wolf, Coleen Sweeney, Carol Santalcuia, Jason Gottlieb, Chris McCarthy, Kip Durney, Jim Rawson, Debra Barrath, and many, many more.
Changing the culture of healthcare takes a village of the committed, personally accountable, energetic, loving and audacious. I love these change agents!
Please join us on March 24th 20:30 EST (8:30 pm) on Twitter for a tweetchat #hcldr
Grassroots Change + Personal Accountability in Healthcare.
Pecha Kucha comes to IHI 26 Forum
Posted: December 11, 2014 Filed under: Change, Disruptive Behavior, Health and Care Radicals, Heretic, Leadership, Making a Difference, Pecha Kucha, Personal Accountability | Tags: Accountability, brave, culture of safety, Healthcare, Leadership, patient safety, speaking up, taking risks Leave a commentPecha Kucha!
“Bless you!” were the first words out of my mouth when I heard someone say peachakoocha during this week’s 26th annual Institute for Healthcare Improvement (IHI) Forum in Orlando, FL. On hearing the word, my 12-year-old daughter thinks it sounds like the name of a Pokemon character…
Weird word = wonderful experience
In a conference environment that can be all too often filled with long-winded PowerPoint presentations with presenters reading slides, this was an energizing and welcome change.
“PEH–cha KOO-cha,’’ is the English pronunciation, of what appears to be a rough translation of the Japanese word(s) for “chit chat’’. Picture an event akin to a poetry slam. A Pecha Kucha is where subject matter experts get together to share their work, opinions and beliefs, and get to hear from others. A fast paced opportunity to share, learn and be inspired.
Pecha Kucha started in 2003 in Tokyo and has since migrated to almost every country in the world. Originally designed to share ideas in design, architecture and photography, it has apparently now come to healthcare. There are now Pecha Kucha ‘nights’ in more than 300 cities around the world.
How does this work?
The Pecha Kucha at this weeks IHI meeting was hosted by Helen Bevan, Chief Transformation Officer for NHS Horizons Group (UK) who acted as host and ‘race marshal’. She explained to the audience what would happen, then welcomed each presenter to the podium, and then asked, “are you ready?”, setting their slides running for the ensuing sub seven minute presentation (6 minutes, 40 seconds)…
Presenters — there were 8 of them at the IHI — shared and narrated 20 slides for 20 seconds that “auto-ran”, meaning the presenter had no control over slide advancement, the slides roll…
The 20 x 20 format is at the core of a Pecha Kucha. The emphasis here is on speed! Can’t keep up, then you’re likely not ready for this rapid fire onslaught of ideas and inspiration.
What we witnessed at the IHI Forum was a Pecha Kucha focused on the theme of “my hope for the future of healthcare”. These were inspiring stories of why each presenter had been called to make a difference in healthcare and provided insights into specific projects that each of them were working on. Beautifully inspiring, brave, personal stories of commitments to lean in and make health and care safer, more accessible and more relationship driven; the triple aim is alive, well and thriving!
A refreshing change at a terrific conference. I commend Helen for leading this and congratulate the IHI for welcoming this imitation of a clearly different approach to sharing, learning and inspiring.
I’m a Pecha Kucha fan!

Check out this Pecha Kucha Storify
Numberless diverse acts of courage
Posted: July 31, 2014 Filed under: Health and Care Radicals, Heretic, Human error, Leadership, Learning, Safety | Tags: brave, Communication, culture of safety, Healthcare, hospital safety, Leadership, Lessons learned, patient safety, speaking up, taking risks, Telluride Summer Camp 3 CommentsYesterday afternoon the faculty and students at the “Telluride-East” Patient Safety Summer Camp visited Arlington National Cemetery.
As we paused for some reflections from our leaders Paul Levy and Dave Mayer I was overcome by the scale of what presented itself in the form of field upon field of white grave markers.
Poignant words reminded those gathered that we were indeed standing on hallowed ground and that many have given, and continue to give, the ultimate sacrifice. A sobering reality is that there are between 25 and 30 new burials every day at the cemetery.

Following our time of reflection I took a walk to reflect on the sacrifice, loss, and scale of what lay beneath me. 400,000 markers of lives once lived, now at rest.
In a recent piece of research published in the Journal of Patient Safety it is estimated that more than 400,000 hospital deaths are attributed to preventable harm. Put another way, since August 2013 more than 400,000 mothers, fathers, brothers, sisters, sons and daughters are no longer alive as a result of harm that could have been prevented with better designed systems, more situational awareness, and other proven human factors and safety science approaches in health care.
I think these numbers are becoming “noise” for many leaders in healthcare, we have heard the numbers and yet still choose not to make the different decisions and the difficult choices. We disassociate from the difficult reality because we don’t “see” the totality of what we are doing.
The grave markers stopped me in my tracks, a visual reminder of what we are doing every year in healthcare by tolerating variation, blaming people, doing the same things over and over and expecting different outcomes.
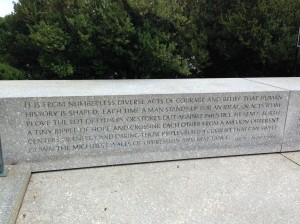
My walk took me to the Kennedy family grave site. Off to the side of the eternal flame is a Robert F. Kennedy quote that really resonated with the work we are doing with the faculty and students at Telluride-East:
It is from numberless diverse acts of courage and belief that human history is shaped. Each time a man stands up for an ideal, or acts to improve the lot of others, or strikes out against injustice, he sends forth a tiny ripple of hope, and crossing each other from a million different centers of energy and daring, those ripples build a current that can sweep down the mightiest walls of oppression and resistance.
Robert F. Kennedy, South Africa, 1966
This quote captures what I will leave this time of learning and sharing with, and what I urge the students, residents and faculty to find the courage to continue doing…
- Lean in and keep speaking up to improve safety; these are the “numberless diverse acts of courage”
- Believe in yourself and the difference you can make
- Stand up for what you know is right and stand up for those less brave and courageous than yourself
- Speak up, even when your voice quivers and your hands shake. Speak up for patients, the ones you care for, know and for the one’s you dont…
- Most of all, send forth a “tiny ripple of hope”. These ripples will build to a current. These ripples will make care safer
- By thinking and acting differently, by bravely speaking up and taking a stand we will sweep down what often feels like a mighty wall
I commit to making ripples and I urge my new found colleagues and friends to do the same.
Make ripples. Ripples save lives, ripples make care safer.
You promote what you permit
Posted: July 25, 2014 Filed under: Disruptive Behavior, Health and Care Radicals, Heretic, Leadership, Patient Experience, Safety, Workplace Culture | Tags: brave, culture of safety, Healthcare, Leadership, speaking up 1 CommentI recently spent a day with a number of senior clinicians all working in an environment that is permitting pockets of disruptive, unprofessional, and quite frankly dangerous behavior amongst caregivers. The last conversation of the day ended with a chilling reminder that we still have much to do, “The problem is that for too long, to be successful in academic medicine, you haven’t needed to be polite, professional and well mannered…”
Last night I read a headline that really grabbed my attention…
Why disruptive docs may not be so bad after all
Here was my reply:
I will start by saying that there is, in my mind, absolutely no place whatsoever for a disruptive (rude, hostile, ill-mannered, bad tempered) anyone in a safe, efficient, patient centered, healthy, just healthcare environment. Let’s not limit this to physicians…
I am sick and tired of hearing that being a technically excellent clinician and being a decent, respectful, polite human being are somehow mutually exclusive. They are not, and to suggest otherwise is disrespectful to the enormous number that are.
Please don’t suggest that organizations committed to improving the experience of those they serve are “getting rid of disruptive docs…” as an approach because they now have dollars tied to HCAHPS performance. This is a gross over simplification.
I’d offer that any healthcare organization that hires and retains mean, disruptive physicians (or anyone else) is complicit in creating a dangerous, un-just, unreliable work environment, not simply a less than ideal patient experience.
We need to start changing the conversation, raising our standards and expectations, and demanding more of one another. A world class, safe, reliable, effective experience is within our reach, but only if we stop confusing experience with “nice” and start holding ourselves and our colleagues to not only the highest technical standards but also high behavior standards.
I understand that we need to be mindful of the words we use, and am enthusiastically open to the idea that we need to lead with more “healthy innovative disruption” as we work to improve the safety and delivery of health and care. (Note the great work done by Helen Bevan and colleagues at the NHS with the notion of being a rebellious health and care change agent). But to suggest that disruptive behavior, in the way this article does, is somehow OK, and furthermore actually has a place in our healthcare environment, is reprehensible.
I’d love to hear your thoughts.
I’m sick and tired – but far from done!
Posted: July 17, 2014 Filed under: Health and Care Radicals, Heretic, Leadership, Learning, Safety, Uncategorized, Workplace Culture | Tags: brave, culture of safety, Leadership, patient safety, speaking up, taking risks 5 CommentsI am an optimistic person that believes that there are plethora hospital leaders doing the very difficult work of changing healthcare to make their cultures more effective, healthy, transparent, more reliable and less variable. I witness examples of these heroes every single day.
So before I take a little time to rant, let me explain… I work with healthcare leaders that are committed to learning from the past to improve the future, with data as their driver and compass. It is not easy work, per se (let’s be clear, it’s also not the front line care of patients), but it is work that I absolutely love! My reality is that what I do for work is a calling; and so my personal opinions are inherently woven into the work I do, I cannot unravel them.
I tell you this part as explanation, and part introduction; please know that I will never reveal the names of those I reference and would ask that your assumptions be kept to yourself. Needless to say, I think you’d be surprised…
I am sick and tired of the fact that I see many leaders in health care not being honest with themselves.
Unprofessional behavior is tolerated, expectations remain unclear, variation in practice is permitted, and human error is being allowed to harm patients; all the while telling people that they are the greatest, safest, most efficient healthcare system(s) in the world.
Why this lack of honesty? Is it that we’re afraid, or is it that we don’t know?
Do we not know the answers to safer more reliable, transparent, less costly care?
If we don’t know, are we embarrassed to admit that we lack the knowledge?
Are we afraid that if we stop supporting and promulgating the structures, systems, processes, excuses, and people that result in our current dangerous reality, that this will be an admission of past guilt? Are we afraid of the difficult conversations and actions that will be needed to lead a different organization?
I think it’s a combination of embarrassment, fear and a multitude of other deeply held attributes that many smart, well educated professionals have a difficult time “owning” and acting upon.
Let me be clear, I don’t think this is a knowledge gap. Other industries are way out in front of us with their use of technology, their speed to change long held approaches that no longer work, and their desire and ability to learn from others. Many hospitals have taken the lead and are modeling that you can hire for ‘fit’, support daily safety huddles and commit to a goal of “zero preventable harm”, just as a start.
I think we’re afraid of the reality that if we fess up to the fact that we have tolerated bad behavior, poor performance and mediocrity for so very long; that we will have to be vulnerable, naked, open to criticism, and honest with ourselves that yesterday we tolerated and did things that are no longer OK today…
So I have a challenge for myself and fellow healthcare leaders:
Own it.
Start taking personal accountability for who and what your hospitals are. The good (great), the bad, and, the ugly. You are culture!
Own up to the fact that you know who your poor performers are…
Own up to the fact that you may not have articulated your expectations clearly…
Own up to the fact that there are voices of expertise within your organization that you are not listening to…
Own up to the fact that your hospitals culture is staring back at you from your bathroom mirror…
Own up to the fact that if you cannot state “zero preventable harm” as a goal – then, by definition, you have agreed to hurt someone’s loved one in a way that could have been prevented…
Own up to the fact that you got into this because you want to make a difference…
Own up to the fact that you’re tired, over worked, stressed, and that you don’t have all the answers…
Or, leave…
Get out, go home, hang it up, retire! Your colleagues, caregivers, team, patients, community, all deserve better than your dishonesty.
We are surely complicit if we continue to stand by and watch – mute, deaf and blind.
I met with a senior member of a hospitals quality and safety department last week, he confided in me (after looking over his shoulder to make sure the door was closed) that his very reputable AMC doesn’t have the leadership “strength” to state that ‘zero preventable harm’ is their goal. He’s embarrassed and afraid to challenge his CEO.
I met with a senior management team that wanted me to know (after I’d found trash lying on the floor of their lobby, that they had walked past and ignored, and I suggested they ‘pick up trash’) that they “have people to do that…”
I hear leaders tell me that they know that their high revenue producing, senior position holding, research leading, long tenure physician colleagues are abusive bullies, and yet they are still employed, practicing and getting their annual bonuses…
These are choices, and my challenge is for us to make different choices.
My challenge comes with a promise…
My promise, is to keep asking difficult questions, pushing for the right answers, and encouraging and coaching healthcare leaders to be brave. Brave to ask when we don’t know, brave to admit that we made a mistake, and brave to reach out and request help.
I for one am not afraid. Apprehensive and nervous, for sure. Apprehensive that my comments will be seen as negative, accusatory and blaming, and nervous that this sentiment will be seen as one more heretic in the noisy world of working to improving safety and become more reliable and excellent.
But when I think about who we are harming, who we hurt every day in the spirit of “health” and “care”, I am not afraid. When I hear the stories of burned out, stressed, under resourced care giver friends and colleagues, I am not afraid. I’m buoyed, inspired and deeply moved by the memories of people like Michael Skolnik, Josie King, Lewis Blackman, and Jerod Loeb; people I never knew, but people who deserved so much better from the cultures that surrounded them and that were meant to take better care of them.
I am also encouraged and inspired by the health and care radicals (leaders at all levels of their organizations) that are making a difference and inspiring their colleagues to think differently, act differently, be transparent, have difficult conversations, model different behaviors and deliver on the promise of “Primum non nocere”.
So my promise is to keep asking difficult questions, pushing for the right answers, and encouraging and coaching healthcare leaders to be brave.
I leave you with challenges and inspirations from three very different healthcare leaders whose work I admire, and who model this mindset of personal accountability;
- “Rock the boat, without falling out” Helen Bevan (NHS guru of innovative change)
- “Ignite the fire within, not the fire underneath” Peter Fuda (Aussie based wicked smart PhD)
- “Proceed until apprehended…” Florence Nightingale